PCS Clinical Competencies for RNs
JCAHO & Dysphagia
The Swallow Screen is one of JCAHO's primary performance measures. JCAHO guidelines state "A screen for dysphagia should be performed on all ischemic & hemorrhagic stroke patients before being given food, fluids, or medication by mouth."
Definition of Screening
- Swallowing screening: refers to minimally invasive procedure that provides quick determination of:
- Likelihood that dysphagia exists.
- Whether patient requires referral for further swallowing assessment.
- Whether it is safe to feed the patient orally.
- IT IS NOT MEANT TO TAKE THE PLACE OF A SPEECH CLINICAL SWALLOW EVALUATION!
Specially Trained RN's Responsibility
- Nursing Swallow Screen will be completed by specially trained NICU & 3W nurses.
- This group of specially trained RN's will complete screens on all patients with ischemic or hemorrhagic strokes regardless of what unit/floor patient is located.
- NICU or 3W specially trained RN will determine, based on results of screen, if patient should remain NPO until Speech Pathology completes clinical swallow evaluation or if patient is safe to begin a PO diet.
Bedside RN Responsibilities
- If patient PASSES nursing swallow screen, bedside RN will page MD to obtain verbal order for specific diet recommended by 3W/NICU RN.
- If patient FAILS nursing swallow screen, bedside RN will page MD to obtain verbal order for Speech Pathology consult for swallowing evaluation. Bedside RN will keep patient NPO for medication, food & liquids until completion of Speech Pathology swallowing evaluation.
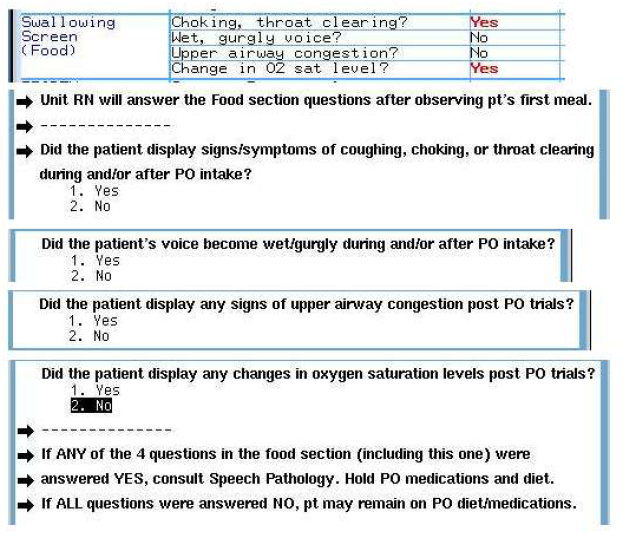
- If patient passes nursing swallow screen & begins a PO diet, BEDSIDE RN will observe the initial 10 min. of the patient's 1st meal.
- After observation, the Bedside RN will answer the following questions:
- RN to answer below questions after 1st meal.
- Did the patient display signs/symptoms of coughing, choking or throat clearing during and/or after PO intake?
- Did the patient's voice become wet/gurgly during and/or after PO intake?
- Did the patient display any signs of upper airway congestion post PO trials?
- Did the patient display any changes in oxygen saturation levels post PO trials?
- Bedside RN Documentation:
 Managing Alcohol Withdrawal with CIWA Clinical severity scale:
Managing Alcohol Withdrawal with CIWA Clinical severity scale:
CIWA-Ar is the Clinical Institute Withdrawal Assesment for Alcohol scale. It is a well-validated 10-item scale. Scores of < 11 indicate mild withdrawal, 16-20 indicate moderate withdrawal, and > 20 indicates severe withdrawal. The 10 items monitored include nausea and vomiting, tremor, sweating, anxiety, agitation, tactile disturbances, auditory disturbances, visual disturbances, headache, and orientation/sensorium.
At Harborview Medical Center, we assess CIWA
- On admission and every 4 hours while awake if CIWA is 10 or less
- Every 2 hours if CIWA is 11-25
- Notify HO if CIWA is greater than 25, continues to increase or does not decrease.
- Notify HO if patient becomes oversedated.
- Discontinue CIWA if scores are less than 11 without medication X 24 hours.
- Orders for medication are symptom triggered, based on your CIWA assessment. Patients without a history of seizures will have only prn orders. The prn order for medication is every 2 hours for a CIWA score of 11 or greater. If the score is under 11, but you assess that medicationneeded to prevent more severe symptoms, you need tocall the doctor for an order. You do not have a prn orderif the CIWA score is 10 and under.
- If patient has a history of Alcohol withdrawal with seizures the option for a fixed medication schedule is available for the physician to order. Routinely given every 6 hours for 48 hours.
- The prn and fixed doses are ordered to be given together if the CIWA score is 11 or greater and the physician has ordered an addition fixed dose. If you assess that the patient will be oversedated with that dose or if the CIWA scores are trending down you may opt to hold the prn dose. However, you must completely document the assessment and rationale each time you hold a dose. If CIWA score is greater than 15, IV administration of the ordered medication is preferred.
Clinical Pearls:
- Suspect alcohol withdrawal in every unexplained case of delirium in the hospital.
- Withdrawal syndromes can co-exist or be mimicked by other conditions. Other conditions that cause delirium, tachycardia and tremors must be ruled out. Watch for infection, other drug withdrawal or overdose, hemorrhage, hypoxia or CNS pathology like strokes and tumors.
- CIWA is less sensitive in the brain injured patient with injury related agitation. Discuss the use of the tool with the MD/NP.
- Do not delay diagnosis; treatment is more difficult if delayed.
- ETOH withdrawl has a cumulative effect, if the syndrome is undertreated the next episode will be more severe.
- Lorazepam may be preferred over diazepam in elderly patients and in those with liver impairment.
- Be cautious about treating hypertension as blood pressure will likely decrease once withdrawal is controlled.
- Addiction services and alcohol abstinence counseling should be offered to all patients.
What everyone should know about Procedural Sedation
The most important thing for every nurse to understand is that sedation is a continuum and that nurses must use their clinical evaluation/assessment skills to determine where along the continuum their patient is and where they want them to be.
Here are a few tips for improving your practice in this area:
- If your intent is to give someone a medication for pain or anxiety and it is part of their routine care, then that is minimal sedation and you don't need to follow the sedation procedure. Monitoring and documentation follow the medication administration policy.
- If your intent is to sedate the patient so they can tolerate a procedure, this is moderate sedation (formerly known as conscious sedation). Moderate sedation improves the patient's cooperation with the procedure and allows a rapid return to pre-procedure status.
- Moderate sedation is a drug-induced depression of consciousness during which patients respond to purposefully to verbal commands, either alone or accompanied by tactile stimulation. No interventions are required to maintain a patent airway, spontaneous ventilation is adequate, and cardiovascular function is maintained.
- Commonly used procedural sedation drugs include IV Morphine, Versed (midazolam), Fentanyl, and Ativan (lorazepam). It's important to remember that IV analgesics and sedatives are administered together, the risk of depressed LOC and hypotension is increased.
- Because the risk with moderate sedation is that the patient's LOC will be depressed past the point where he or she can maintain a patent airway (a state referred to as deep sedation), acute care units are required to call the STAT nurse or PACU to give sedation for procedures needing to be done that same day. STAT and PACU nurses have advanced airway management and resuscitation skills to manage a patient who progresses to deep sedation.
- The Anesthesiologist in Charge of the OR can be called at #8800 to arrange for same day anesthesia procedures. The patient's primary service can schedule future procedures that need Anesthesia or sedation by calling the OR Schedule Desk at #6002.
- Education in assessment and care of sedation patients will be offered every 6 months (April & November) and is provided for all nurses giving conscious/procedural sedation.
- NPO guidelines are being enforced now for non-emergent sedation procedures.
- H&Ps are required to be updated with 24hours prior to all sedation procedures. ER physician assessments and admission notes count as H&Ps as long as they have a systems review.
- Patients that do not have a ride home should be monitored for a minimum of 6 hours and a physician's order should be written for their discharge without an escort.
- Patients that receive a reversal agent must be monitored for a minimum of 2 hours from the time the last dose was given.
See the Sedation/Analgesia for Procedures Nursing Procedure available with other nursing procedures on HMC intranet @ hmcweb.washington.edu for more details
Epidural local anesthetic
Epidural local anesthetic medications (bupivacaine, ropivacaine) provide pain relief by blocking nerve impulses.
Pain nerves are most sensitive to local anesthetics. This means that a good epidural can provide analgesia without affecting muscle power or other types of sensation (this is the goal). However, all nerves in the area of coverage are susceptible and the effects usually occur in the following order.
- Decrease of pain
- Decrease of sensation
- Decrease of muscle power:
*Impaired sympathetic nervous system function can also occur (often causing hypotension).
*Larger doses have more effects on the nerves resulting in a larger risk of side effects
Some of the possible side effects are (call PRS):
- Skin breakdown and urinary retention
- Hypotension
- High sensory or complete motor block
- Local anesthetic toxicity (watch for CNS changes, arrythmias, hypotension)
Routine monitoring is essential!
Monitoring includes:
- Blood pressure and pulse (watch for hypotension)
- Sensory level (use an alcohol swab or ice and note upper boundary of level (i.e.mid-nipple line, umbilicus, groin).
- Motor strength (ability to bend and straighten knees)
Q 30 min x 2hr, Q1 hr for 4 hours, then Q 4 hours, after start of infusion and as ordered when local anesthetic concentration or rate is increased.
- Pain level Q 4 hours while awake
Epidural Opioid:
- Epidural opioid analgesics (preservative free morphine and fentanyl) modify pain nerve impulses by diffusing past the dura and binding to opioid receptors in the spinal cord. They also produce analgesia by being absorbed systemically (much like an intramuscular injection.)
- Respiratory depression can occur when opioids are given in the epidural route. The timing of this opioid related side effect is sometimes unpredictable.
- When epidural opioids are given, monitoring includes respiratory rate every one hour for the first 24 hrs, then Q 4 hrs.
Epidural Abscess
Epidural Abcess is a complication that requires prompt recognition and proper management to avoid potentially disastrous complications. It can occur as a complication of an epidural catheter.
- Strict asepsis is maintained whenever accessing the epidural system!
- Epidural filter is a standard part of the system and will prevent some bacteria from entering the epidural space. All medications should go through the filter.
- Cleanse connections with alcohol and then allow drying prior to opening the system.
When caring for a patient with an epidural:
- Check that the epidural has not migrated (check catheter markings at the skin) every shift and as needed.
- Do not change the epidural dressing. (Document and notify PRS if the site has been exposed.)
- Turn patient every 2 hours and assess skin frequently.
- Maintain IV access is for 24hours after last epidural medication is administered.
- Label infusion pump, tubing and catheter with "Epidural."
- When injecting opioids into the epidural space make sure they are preservative free. Remember to aspirate. (If blood or CSF is found, discard aspirate and notify PRS.)
- If extra bupivacaine is ordered, it is administered by temporarily increasing the rate on the infusion pump for a limited time and volume. An example of an order is "Increase the infusion rate to 60ml per hour to infuse 10ml, then continue infusion rate of 12ml/hr". Remember to change from "infuse all" to the volume prescribed ("10ml" in this example).
- Maintain strict asepsis.
Which patient needs a spine assessment?
- 70 y.o. man w/ metastatic prostate CA. Admitted with new onset bilat LE weakness.
- 82 y.o. woman fell in her bathroom yesterday. Admitted from the ER last night with R hip fracture and a C/O neck tenderness. Initial ER C-spine film showed no fracture. She is wearing a Miami J collar and is on partial spine precautions.
- 6 y.o. admitted after a 15 ft fall. He returned from having a head CT with an" incidental finding" of aneurism at C2. He has no fractures.
- If you answered "all of them", you are correct. Most of us know that patients with spinal TRAUMA require neurological monitoring. But trauma is not the only mechanism for neurological damage.
- ANY type of spine pathology can lead to nerve injury or compression. Deterioration in the exam can mean a medical emergency!
- Possible interventions include surgical decompression or steroids.
The HMC standard of care is to perform a spine assessment on any patient with spine pathology.
My patient needs a spine assessment. How do I start?
- Start with motor assessment. Most people who are able to follow simple directions can comply with a motor assessment.
- Remember that the motor score reflects strength, so the patient must give their best effort.
- Start by asking if the patient can lift off bed. If he cannot, his score is 0, 1 or 2. If he can, his score is 3, 4 or 5.
0= No movement
1= Visible muscle contraction but NO movement
2=Can move on bed, but unable to lift
3=Can move or lift off bed, CANNOT overcome resistance
4=Can move or lift against resistance, NOT full strength
5=Full strength
- What about the sensory assessment?
- Starting from the foot, touch the patient with an object, testing ability to feel touch (can you feel this?) and then identify sharpness (does it feel sharp or dull?)
- What if my patient was able to feel light touch but didn't feel sharp?
- Nerve fibers conveying specific forms of sensation (tactile and pain) follow separate pathways in the spinal cord. Document: "Impaired".
0=Absent
1=Impaired (includes increased, decreased or tingling)
2=Normal
3=Not tested
- Is that all?
- Depending on the level of spinal cord injury, respiratory, bladder and bowel function can be affected. Simple assessments of these status areas are also included in the routine spinal assessment.
Last modified: 7/25/2008 9:53 AM