PCS Clinical Competencies for RNs
A complete wound assessment plus accurate documentation of that assessment are vital components of the wound care plan. Documentation provides a record of the wound status on which changes to the care plan are based.
- To document wound healing or deterioration, a complete wound assessment, including measurements, should be done initially upon admission, or when the wound is first discovered, and at least weekly thereafter.
- Wound assessments, documentation, and treatment plans should only be performed by an RN, MD, PA or ARNP. An MA may assist with wound care, or follow a treatment protocol, if directly supervised by an RN, MD, PA or ARNP.
- At Harborview, we have picked Wednesday as "Wound Wednesday" – the weekly day to measure all wounds.
- In outpatient clinics and ED areas, wounds should be completely assessed with each patient visit.
- Description of the wound should be documented with each dressing change, and changes to the wound care treatment plan should be implemented according to the condition of the wound.
- All wounds that develop while the patient is at Harborview require that a PSN report be filed.
A complete wound assessment should include five key elements:
- Nutritional status
- Smoking status
- Wound etiology
- Wound appearance
- Pain
The ability to heal is dependent upon adequate nutrition. A wound will not heal, and will often deteriorate, if a patient does not have adequate protein and calorie intake to form new tissue.
- A prealbumin level >19 mg/dl is an accurate measure of adequate protein stores to heal a wound. (Serum albumin is not as reflective of the patient's current condition, and may be affected by hydration status, renal function, and infection.)
- If a patient is expected to be NPO for >24 hours, encourage tube feeding or TPN to decrease chances of depleting patient's protein stores.
- If patient is taking p.o., and it is not medically contraindicated, encourage high protein food sources such as milk products, meat products, legumes, and shakes.
- Unless a patient has a known deficiency, a multivitamin is sufficient dietary supplement.
Numerous studies illustrate that smokers experience longer healing times (one study documented 2.5 times longer than non-smokers) and more complications than non-smokers. In a study published in the Annals of Surgery, July 2003 by Sorensen, et al, smokers had a higher wound infection rate than non-smokers and 4 weeks of abstinence from smoking reduced the incidence of wound infection. Encourage the patient to learn about smoking cessation through classes offered by the Patient and
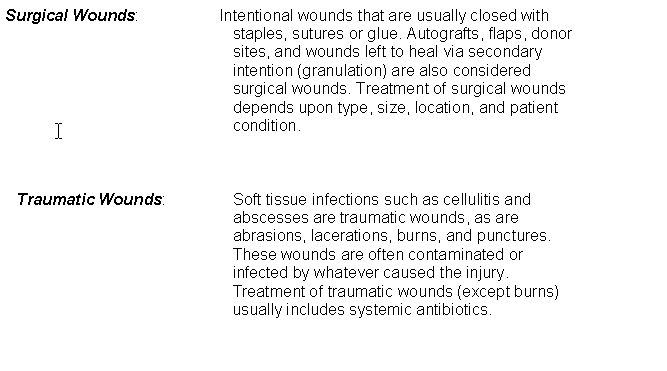
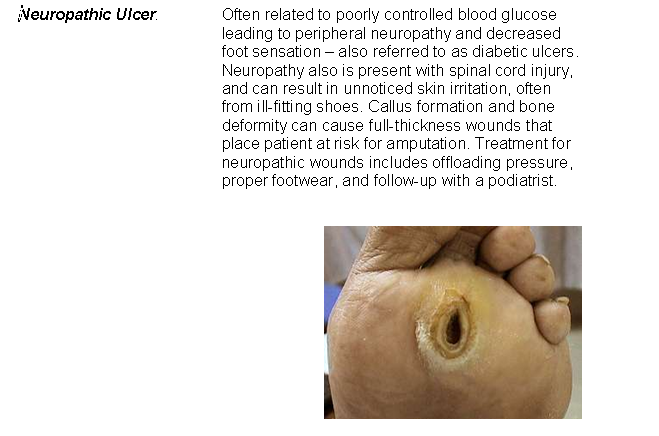
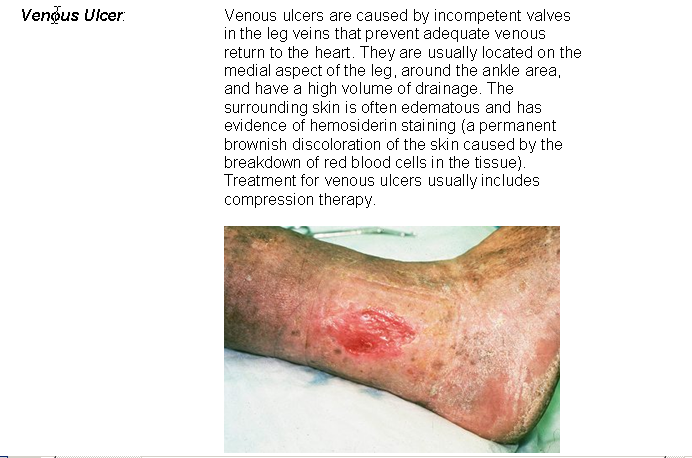
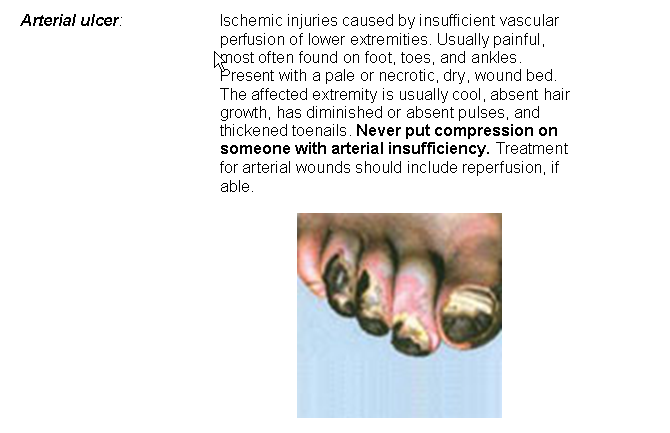
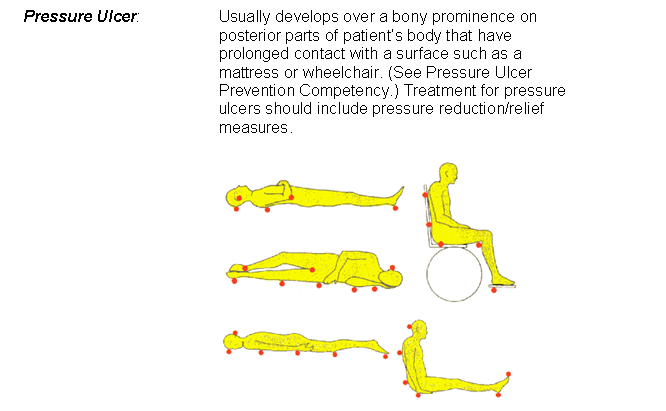
Wound etiology is a very important component of wound assessment – if factors causing the wound cannot be controlled or avoided, it may be difficult or impossible to heal the wound or prevent it from deteriorating. To assess wound etiology, it is important to understand the characteristics of different types of wounds.
Assessment of a wound must include:
- Location
- Size
- Depth of injury
- Undermining/Tunneling
- Wound base tissue
- Drainage
- Condition of periwound tissue
Location: describes where each wound is located on the patient's body. For each wound there should be a corresponding wound macro modified in CIS.
Size: Describes the height, width and depth of each wound recorded in centimeters. Measurements should be included with wound documentation on admit (or upon discovery, if nosocomial), weekly, and within 24 hours of discharge.
Depth of injury: Describes the level of tissue destruction. Partial-thickness wounds describe injury to epidermis down through dermis; full-thickness wounds describe injury that extends through dermis into underlying tissues or structures. Pressure ulcers are staged according to level of tissue destruction. (See Section 2: Pressure Ulcer.)
Undermining/ Tunneling: Describes the depth and location of the undermining/ tunneling in a wound. Undermining indicates tissue loss under an area at the margin of the wound. Tunneling describes a sinus tract in one direction. The depth is recorded in centimeters at its deepest level. The location of the undermining or tract is described using the position in relation to the face of a clock. It compares where the undermining/ tunneling is in relationship to the patient's head. For example, the patient's head is considered 12 o'clock, and feet would be considered 6 o'clock.
Wound base tissue: Describes what the wound base looks like in terms of tissue healing. Some examples would be: granulation, epithelialization, slough, eschar. Often documented as percentages – ie. 30% slough, 70% granulation.
Drainage: Describes the color, consistency, odor and amount of drainage coming from the wound. The amount of drainage is a subjective approximation. A moist wound where the drainage is contained on the wound bed only – tissue appears shiny or moist - would be described as "Scant". Drainage which requires that the dressing be changed more often than normally expected would be described as "Large."
Condition of the periwound tissue: Describes what the tissues around the wound look and feel like. For example: Is there erythema, maceration, bruising, breakdown, or swelling in the surrounding tissues? These could indicate infection, or potential for further tissue breakdown. Treatment of periwound skin should be included in the wound care plan, if applicable.
Pain is also an important component of wound assessment. Typically, wounds that are acute, partial thickness (with intact nerve fibers), infected, or due to ischemia are usually associated with increased pain. Pain can also occur with full-thickness chronic wounds.
Ask the patient if they are having pain with wound care. The wound care treatment plan should provide for adequate pain control. In addition to the use of analgesics, the most effective pain management often involves a combination of techniques designed to eliminate or control the source of pain (i.e. pressure, movement, exposure, edema, or manipulation of the wound). Provide analgesia as needed and appropriate. Wound pain between dressing changes can be controlled or eliminated by choosing dressings that cover the wound bed and exposed nerve endings, that adhere as little as possible to the wound bed, and that leave minimal residue behind.
Pain management requires planning to coordinate timing of analgesics for peak effect during wound care. In addition to systemic analgesics, consider obtaining physician order for topical application of 4% lidocaine solution for localized pain reduction. Allow adequate time (15-20 minutes) for lidocaine to be absorbed before beginning wound care.
Documentation:
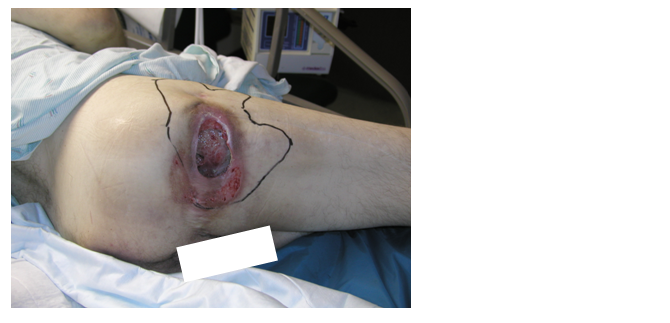
Scenario: 44 Year-old paraplegic male with a six-month old Stage IV right ischial pressure ulcer. The wound care dressing has been Kaltostat rope covered with Duoderm that has been ordered to be changed every 3 days. The wound has yellow, thick drainage. Undermining noted from the patient's upper posterior thigh to mid buttocks, which measures 4.3 cm at its deepest. New partial thickness breakdown due to maceration noted on posterior aspect of surrounding tissue.
The following is an example of documenting the wound assessment in CIS.
1. Right Ischial Stage IV Pressure Ulcer is added to the Problem List in both the Acute and Intensive Care areas.
2. On the Acute Care Unit, modify form to add cell for the specific wound under the Assessment Tab on CIS:
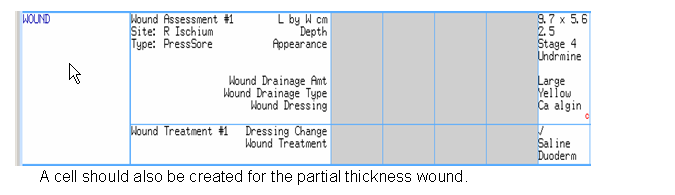
3. Narrative documentation about the wound is done on both the Intensive and Acute Care Units.
- On intensive care units, narrative documentation about the wounds is done in the "Integumentary" section under the ICU Assessment. Modify form to add cell for each wound.
- On acute care units it is done under Case Note as a Nursing Progress Note.
- In the ED and Clinics, wound care documentation is done in ORCA.
The complete narrative documentation about these wounds would look like the following:
Patient T12 paraplegic with chronic Stage IV pressure ulcer to right ischium. Right ischium insensate related to paraplegia. Patient did not require pain medication prior to wound care.
Undermining from 8-11 o'clock at a depth of 4.3cm. Wound bed measures 9.7 x 5.6 x 2.5cm and is fully granulating with no observable necrotic tissue. Large amount of yellow drainage with no odor noted. Surrounding tissue with brown hyperpigmentation and erythema. Area of partial thickness breakdown measuring 7.8 x 1.2cm to the posterior aspect of the surrounding tissue. Scant amount of serous drainage.
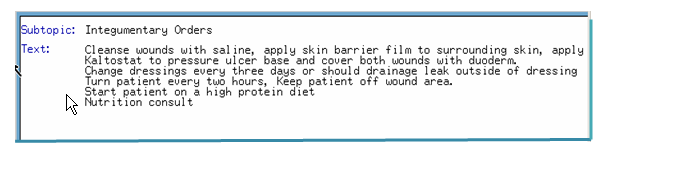
Wounds were irrigated with normal saline, and No Sting Skin Barrier film applied to surrounding skin to prevent further breakdown from maceration. Calcium alginate rope to wound cavity and undermining. Covered with a hydrocolloid dressing. Hydrocolloid dressing also applied to partial thickness breakdown area. Plan to change dressing in 3 days or prn leaking.
Patient instructed in importance in staying off wound areas and limiting sitting in a wheel chair to one hour. Verbalizes understanding.
Pre-albumin 12, nutrition consult pending. WBC within normal limits and patient afebrile. Will monitor erythema.
Dr Smith informed about new skin breakdown area, orders received.
4. In the intensive Care Units, wound care orders are documented in the patient's medical record and transcribed in "Integumentary Orders" under ICU Assessment.
In acute care units, wound care orders are documented in the patient's medical record and transcribed to the Kardex.
An important part of wound documentation includes evaluation of the treatment plan. Statements regarding progression or healing of wound should be included in evaluation. Any patient or caregiver teaching should also be documented.
Consider the following elements when providing health education:
Smoking cessation: Wound healing is negatively impacted in patients who smoke. Encourage the patient to attend a smoking cessation class. Refer patients to the Patient and
Diabetics and blood glucose regulation: Wound healing is negatively impacted in patients with abnormal glucose levels. Stress the importance of regular blood glucose monitoring and regular mealtimes.
Activity: Depending on the wound etiology and location, the patient may need to increase or decrease activity. For example, excessive walking should be limited for a patient with a diabetic ulcer on the plantar surface of the foot and the patient with a venous stasis ulcer should be encouraged to walk in order to promote venous return.
Symptoms that necessitate emergent care: Instruct the patient to seek immediate care if they experience fever, chills, increased warmth to the wound or surrounding tissue, or purulent drainage, pain increase or decreased sensation to an extremity with a wound
Bathing practices: Instruct the patient to coordinate with dressing changes with daily bathing routines.
Patient's lifestyle: Evaluate the treatment plan with the patient's lifestyle and modify the plan for an optimal outcome. Consult a SWAT (Skin and Wound Assessment Team) nurse for types of dressings which require less frequent changing.
Last modified: 5/24/2006 8:34 AM