Clinical Competencies for AACS RNs
A PSN report must be filed for all wounds, including pressure ulcers, which develop while the patient is at Harborview.
Beginning
A pressure ulcer develops from constant pressure applied to skin over a bony prominence when pressure reduction measures (such as shifting one's weight) have not been taken to relieve the constant pressure. Blood flow into the area in not available causing a lack of oxygen and nutrients to the tissues. Nor can the lymphatic system can not function effectively in removing waste products. This causes localized tissue damage or necrosis. Pressure ulcers are found in an individual where mobility is limited or absent or the person's cognitive ability does not support adequate movement.
Risk Factors for developing a pressure ulcer include individuals with the following:
- Impaired sensory perception where the person lacks the mental ability or neural connection to understand and respond to pressure related discomfort.
- Immobility where the person lacks the ability to move or is confined to the bed or chair.
- Frequent moisture exposure which causes maceration of the skin as do irritants in the liquid.
- Friction/ Shear, from two surfaces moving across each other, reduces tissue tolerance to pressure by abrading and damaging the skin
- Poor Nutrition and/ or dehydration are associated with altered tissue regeneration and the inflammatory response.
- Age - Elderly and infants/young children are more at risk related to thinness of their skin and less ability of their immune system to fight off an infection,
Other names for pressure ulcers include pressure sore, bed sore and decubitus ulcer.
The Braden scale is a validated risk assessment tool used to identify individuals who are at-risk for developing pressure ulcers. The scale has six general risk factors in individual CIS cells:
There is a pop-up assessment scale for each risk factor on the Braden scale. The nurse selects the descriptor on each pop-up scale which best describes the patient status at the time of assessment. A numeric value is give to each chosen descriptor.
Once there is numeric value for each of the six general risk factors, CIS will generate a total Braden Score. A total score 16 or less on the Braden Score identifies individuals who at high risk for developing pressure sores. Low scores in any of the risk factors indicate where interventions would need to be focused to decrease the risk.
Interventions would need to be implemented to decrease the risk of developing a pressure ulcer in patients with a score of 16 or less on the Braden Scale. The nurse would focus the interventions to meet the individual situation, needs of the patient and low scoring areas on the Braden Scale. To foster collaboration and reduce the risk of pressure ulcer development, both in hospital and at home, patients and their caregivers would need to be taught these interventions.
1. Interventions for a low score in "Sensory/ perceptual" on the Braden Scale
- Correct causes of disorientation, sleep deprivation and over-sedation
2. Interventions to treat a low score in "Moisture" on the Braden Scale
A. Perspiration
- Treat cause such as infection, fever, estrogen withdrawal
- Decrease room temperature as condition allows
- Increase air flow or ventilation in the room, as appropriate for the patient
B. Urinary incontinence
- Identify and treat urinary tract infections
- Correct environmental factors: easy to remove clothing; call-light, urinal, bedside commode, bedpan placed at close reach of the patient
- Normalize blood sugar, high blood sugars cause diuresis
- Schedule diuresis causing medications at a time when the patient, caregiver or staff is most able to management urine output
- Schedule toileting and assess bladder for complete emptying for those who have neurogenic bladders
C. Diarrhea
- Identify and treat bowel infections
- Eliminate bowel irritants, such as coffee, or food sensitivities from diet
- Consider need for lactobacillus after antibiotic treatment
- Cleanse the skin soon after it was soiled
- Add bulking agents (such as fiber, banana flakes, rice, tapioca or potato)
- Contain wetness when appropriate with rectal pouches, rectal tubes, catheters and Ostomy pouches
- Schedule bowel program to break the diarrhea/ constipation cycle and for those who have spinal cord damage.
D. Wound drainage
- Use high absorbency dressings, such as Kaltostat or Biatin, to wick drainage away from the skin
- Use a Pouch over wound or puncture sites to collect constant or a very large amount of drainage, as needed
E. Additional Interventions to manage moisture or damage to skin
- Protect skin from wetness with use of skin barrier cream or film
- Avoid using hot water as it damages the skin
- Use mild cleansing agent that minimizes irritation and dryness of skin
- Use of moisturizer for dry skin
- Maintain moisture content in environment above 40% to decrease dryness
- Reposition patient to promote drying
- Frequently check gowns, linen and pads for wetness and change when wet
- Increase drying by increasing air flow with an air-surface bed
- If adult briefs are utilized, leave open-to-air when in bed.
3. Interventions to treat a low score in "Activity" on the Braden Scale
A. For patients confined or spending most of time in bed
· Turn patients every two hours for those who are in bed
· Heels off the bed at all times.
o CAUTION: Air surface beds do not eliminate the risk of developing pressure ulcers to the heel
· Avoid placing patient directly on the trochanter and shoulder. Flex hips to 300 and use pillows to support patient's back, between legs and under patient's head per their preference.
· Avoid massaging skin over bony prominences as that causes capillary breakdown, this would include scrubbing or rubbing during bathing
· Use moisturizer to minimize dry flakey skin
· Consider use of protective dressings (such as Tegaderm or ultrathin Duoderm), skin barrier film, or protective padding to decrease friction
between skin and linens.
B. For patient confined or spending most of time in a chair or wheel chair
- Reposition patients in a chair every hour
- For patients who are aware of their surroundings and sensate, teach them to do pressure releases every 15 minutes.
- For those patients who are either not cognitively aware or insensate, reposition their seat position every hour. Teach care givers to do the same.
- Approved pressure relieving cushion made of gel, air, foam or a combination can be a valuable aid for those who unable to shift their weight every 15 minutes.
CAUTION: Do not use inflatable or ring-shaped devices, such as donuts, as these put increase pressure to skin areas in contact with the devices.
4. Interventions to treat a low score in "Mobility" on the Braden Scale
- Consider pressure reducing or limiting mattresses or overlays for those at high risk or who have multiple wounds in contact to bed surface.
- Reposition patient every two hours utilizing a posted turn schedule
- Position trapeze so cognitively aware patients can assist with moving
- Involve physical and occupational therapy early in the patient's care to maintain and improve the patient's strength, flexibility and mobility.
5. Interventions to treat a low score in "Nutrition" on the Braden Scale
- Maintain or promote a balanced diet including adequate protein and calories intake
- Promote a nutrition consult so that a multidisciplinary effort can be made to maximize the patient's nutrition
- Teach patient and care givers about the importance of a balanced diet
6. Interventions for a low score in "Friction/ Shear" on the Braden Scale
A. When the patient is in bed
- Avoid positioning head of bed higher than 300 incline to prevent sliding and associated shear.
- CAUTION: Patient's receiving tube feeding must have the head-of-bed at 300.
- CAUTION: Patients need to have the head-of-bed near 900 or up in a chair for meals
- Use of a footboard, gatch the knee on the bed or place pillows under the lower legs to reduce sliding when head-of-bed is elevated.
- Always use sheets to move and turn patients
- "Lift" patient to prevent dragging of sacrum and heels
B. When the patient is up in a chair
Place foot stools or use wheelchair rests to support feet and minimize sliding
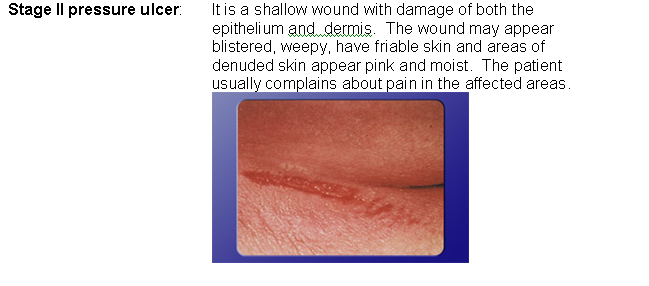
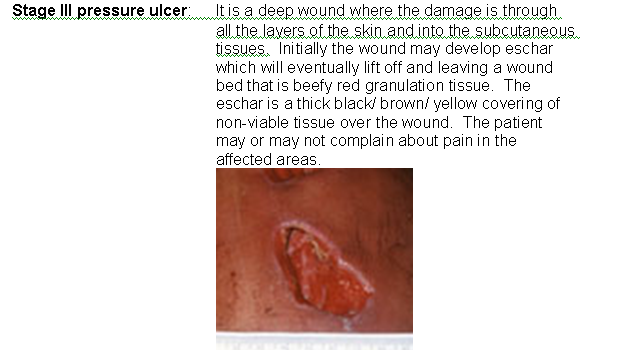
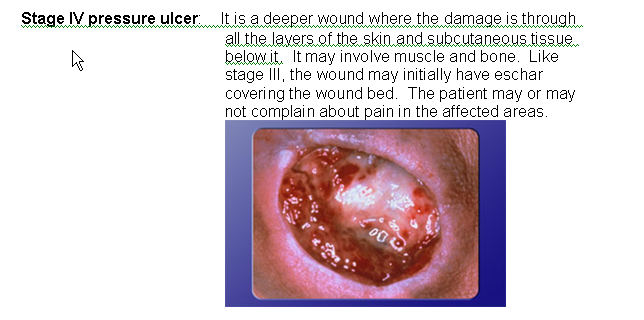
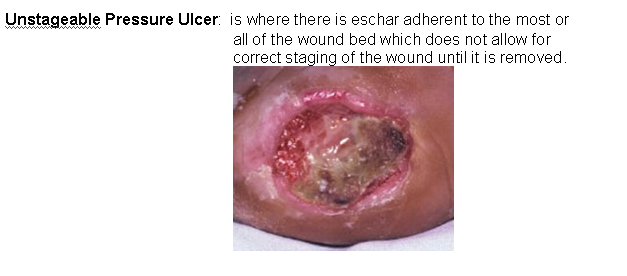
Patients may either come in with a pressure ulcer or, even with our best efforts, develop one in the hospital. Pressure ulcers are staged based on the level of destruction to the layers of skin and underlying tissues. Being able to correctly identification of the stage of the pressure ulcer assists the nurse, physician, patient and caregiver to monitoring its progress, encourage best treatment and take preventative measures.

Last modified: 5/23/2006 2:52 PM